New study tackles chronic kidney disease in the East End community
May 23, 2024
Chronic kidney disease (CKD) is the ninth leading cause of death in the United States according to the National Center for Health Statistics.
An estimated 37 million people in the U.S. are affected by the disease, according to the National Kidney Foundation. Alarmingly, about 90% of those affected are unaware.
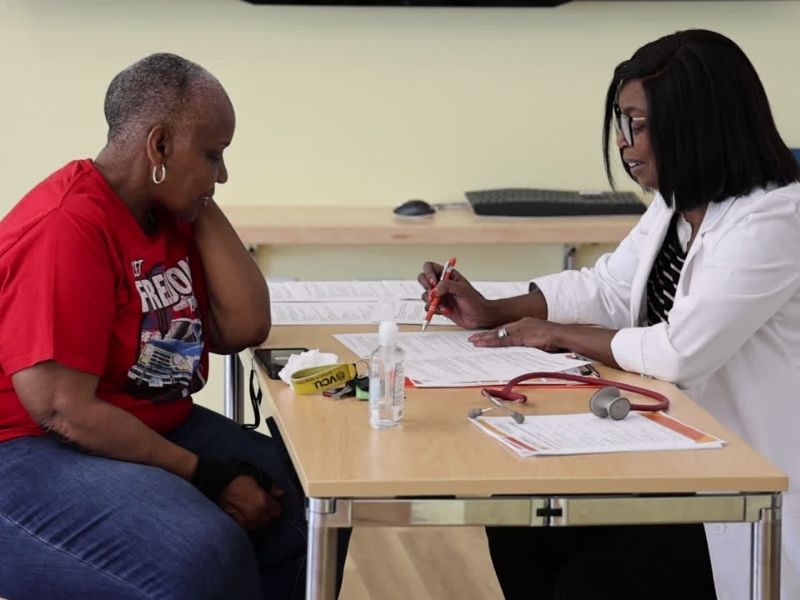
A study being pursued by VCU School of Nursing affiliate researcher Amber Paulus, Ph.D., RN, aims to increase awareness of kidney disease through educational offerings, conducting evidence-based social and CKD risk screenings, and initiating referrals to meet needs among East End communities in Richmond, Virginia—an area identified as having high health disparities.
The study, Designing Equitable Care for Kidneys (DECK): Community-Based Screening for Social Determinants of Health and Kidney Disease Risk Factors, was funded by the National Kidney Foundation and is actively accepting participants.
Paulus spoke with us about kidney disease risk factors, the study and how to participate in a screening.
What are the most common risk factors for developing kidney disease?
I call this the trifecta: high blood pressure, high blood sugar (diabetes), and obesity. Outside of these three primary factors, several other conditions significantly impact kidney disease risk, including:
- Smoking
- Heart disease
- Age over 60 years
- Family history of chronic kidney disease or kidney failure/being on dialysis
- Personal history of acute kidney injury
What are the early signs and symptoms of kidney disease that individuals should be aware of?
Additionally, evidence has shown that minority groups have an increased risk for chronic kidney disease.
The major barrier to addressing kidney disease is general awareness. Because the disease can progress silently and doesn’t exhibit major symptoms until it is advanced, most people don’t realize anything is wrong.
Amber Paulus, Ph.D., RN
Kidney disease is often called a “silent disease” because it can have few or no symptoms. In fact, you can lose up to 90% of your kidney function before experiencing any noticeable symptoms.
As the disease progresses, individuals may experience:
- Muscle cramps
- Loss of appetite
- Swelling in the feet and ankles
- Dry, itchy skin
- Shortness of breath
- Trouble sleeping
- Foamy urine
- Changes in urination patterns (either too much or too little)
What are the primary methods for diagnosing kidney disease in its early stages?
Individuals who have a primary care doctor can be screened for risk factors, ensuring they receive appropriate treatment to prevent chronic kidney disease. Controlling common causes like hypertension and diabetes is crucial. Additionally, two tests can identify kidney disease using blood and urine:
- Blood Test: This test assesses the glomerular filtration rate (GFR), which measures how well your kidneys are filtering your blood.
- Urine Test: This test checks the albumin-to-creatinine ratio. Albumin is a protein that can pass into the urine when the kidneys are damaged.
- Regular screenings and early detection are key to preventing and managing chronic kidney disease effectively.
What are the long-term health outcomes for individuals with chronic kidney disease?
Chronic kidney disease (CKD) is a progressive disease that increases the risk of cardiovascular disease, mortality, and morbidity. It is the 9th leading cause of death in this country. Advanced CKD can lead to:
- Bone and mineral disorders (weak and brittle bones)
- Mental health conditions (depression and anxiety)
- Fluid buildup (swelling in feet and ankles)
- Increased risk of infection due to a weakened immune system
Are there relationships between kidney disease and other chronic conditions?
Yes, kidney disease and heart disease are linked and share common risk factors, including diabetes and hypertension. Each condition can lead to or worsen the other.
What are some of the barriers to early detection and diagnosis of kidney disease in the general population?
The major barrier to addressing kidney disease is general awareness. Because the disease can progress silently and doesn’t exhibit major symptoms until it is advanced, most people don’t realize anything is wrong. Additional barriers to screening for kidney disease include:
- Patient-related factors: Financial hardships, poor health-seeking behavior, and limited knowledge and awareness.
- Healthcare-related factors: Work overload and ineffective communication between patients and healthcare providers.
- System/policy-related factors: Lack of laboratory supplies, lack of primary care providers, lack of guidelines, and poor medical record keeping and documentation.
What does the process of screening for kidney disease involve, how intensive is it, and how frequently do you recommend someone undergo screening?
A basic blood and urine screening takes about 10 minutes, or 20 minutes including thorough education about the findings. Initially, we conduct a test to assess the results, and if an individual’s lab values show evidence of disease, we schedule a follow-up in 3 months to verify that the initial result was not a fluke.
Chronic kidney disease is defined as kidney damage or an estimated glomerular filtration rate less than 60 ml/min/1.73 m², persisting for three months or more. Kidney damage is assessed by detecting albuminuria, which involves measuring a urine albumin-creatinine ratio of ≥30 mg/g (μg/mg). Albuminuria is one of the first signs of kidney disease and, if left untreated, may progress to kidney failure.
How can community-based screenings improve early detection rates for kidney disease?
Community-based screenings can improve early detection of kidney disease by targeting high-risk populations and providing opportunities to access care. The screening is just the beginning; it creates awareness of each individual’s health status. From there, we can build referrals to ensure individuals stay on the path to health rather than waiting for the disease to become significantly advanced.
Once an individual is diagnosed with kidney disease, what are the interventions and how effective are they at managing the condition?
Early detection is the most effective way to manage kidney disease. If detected early, changes to diet and medication can help slow or prevent its progression. Newer drugs, such as SGLT2 inhibitors, are showing promise in protecting the kidneys, slowing the progression of kidney disease, and reducing the risk of death from cardiovascular disease.
Describe the follow-up and referral process for individuals who are identified as at risk or who have kidney disease.
Through the DECK study, we will conduct initial screenings in the community, similar to the ones we are doing this week. Participants will receive their results and a risk score on site. Those whose risk meets clinical referral criteria will be scheduled for a follow-up in 3 months. During this period, we will follow up with participants to address any unmet social needs identified during the screening and make appropriate referrals to community-based organizations.
What have you learned or observed through these community-based screenings?
This is such a needed resource. Every community member we’ve met so far has been identified as having moderate to high risk for kidney disease and needed to be here.
If someone would like to be screened, how can they participate?
They can simply show up at the Health Hub on screening dates. We have had a number of screenings this week and we are working to schedule additional screening dates in the coming month. We are out in the community meeting people where they are and distributing flyers to increase awareness. Individuals who want to participate can call 804-280-6361 to schedule a screening or fill out the interest form to be contacted.